Important Points
- Compared to traditional medications, which are 60-70% effective, advanced laser therapy treatments are 90% effective against stubborn toenail fungus infections.
- Photodynamic therapy, which combines light activation with specialized agents, penetrates deep into the nail bed to eliminate fungus that other treatments can’t reach.
- Nanotechnology-enhanced topical treatments dramatically improve the delivery of medication through the nail plate, increasing success rates even in severe cases.
- Early intervention with technological treatments significantly reduces the time it takes to treat the infection and improves outcomes compared to waiting until infections become advanced.
- Certified Foot clinics offer specialized laser fungal treatments that provide faster results than conventional approaches while minimizing side effects.
If you’ve tried over-the-counter solutions without success, you’re not alone. Advanced toenail fungus infections often resist traditional treatments, leaving sufferers frustrated and embarrassed by persistent discoloration, thickening, and crumbling nails. Fighting toenail fungus can feel like a losing battle when conventional treatments fail.
Thanks to modern technology, there are now more options for treating toenail fungus, especially for those who have not had success with traditional treatments. One treatment that has shown promise is laser nail fungal treatment, which is available at specialized foot clinics. This treatment option is able to penetrate deeper and work faster than traditional treatments, and it has a higher success rate.
More Than Just Looks: The Real Problem with Toenail Fungus
Onychomycosis, more commonly known as toenail fungus, affects nearly 14% of the general population. This percentage increases to over 40% in older adults. While it may seem like just a cosmetic issue, toenail fungus can actually cause pain, limit mobility, and create an entry point for more serious bacterial infections. If left untreated, severe cases can cause permanent damage to the nail and spread to the surrounding tissue.
The Downside of Traditional Toenail Fungus Treatments
Standard treatments often fail to get the job done due to the nail plate’s protective barrier. This thick keratin structure provides a safe haven for the fungus, making it hard for topical medications to reach the nail bed, where the infection thrives. While oral antifungals can penetrate this barrier more effectively, they come with their own set of problems, including a risk of liver damage that necessitates regular blood tests. On top of all this, standard treatments often require lengthy treatment periods—sometimes as long as 6-12 months. Over such a long period, it’s only natural for patients to become less diligent about their treatment, which further decreases the chances of success.
Why You Shouldn’t Ignore Toenail Fungus
It’s easy to dismiss toenail fungus as a cosmetic issue, but it can lead to serious health problems if left untreated – particularly for people with diabetes or weakened immune systems. The fungus can cause the nail to become brittle and crack, and the skin around the nail can become inflamed. These breaks in the skin and nail can allow bacteria to enter the body, which can potentially cause cellulitis or even a bone infection. Plus, the thickened, misshapen nails can create pressure points inside your shoes, leading to painful pressure sores that may not heal well. That’s why it’s so important to treat toenail fungus as soon as possible – especially if you’re at higher risk of complications.
Who’s Most Likely to Suffer from Chronic Infections
There are several factors that significantly increase both the likelihood of getting a fungal infection and the resistance to standard treatments. Adults over the age of 65, for example, have slower nail growth and a weaker immune response, which creates the perfect conditions for chronic infections. Athletes and people who frequent the gym are also at risk due to their constant exposure to fungi in warm, moist environments. Those with conditions that affect circulation, such as diabetes, peripheral vascular disease, or immunosuppressive disorders, are not only more likely to get infections but also have a harder time with conventional treatments due to reduced medication delivery through compromised blood flow. For these populations, technological interventions can be especially beneficial.
Laser Therapy: The Pinnacle of Technological Treatment
Laser therapy is the biggest advancement in toenail fungus treatment in years. FDA-approved laser systems use focused light energy to penetrate the nail without harming the surrounding tissues. This non-invasive method usually needs 2-4 treatment sessions with several weeks in between each session. Studies show impressively high success rates, with almost 90% of patients having complete fungal clearance and healthy nail regrowth, according to clinical data from the Lunula laser system.
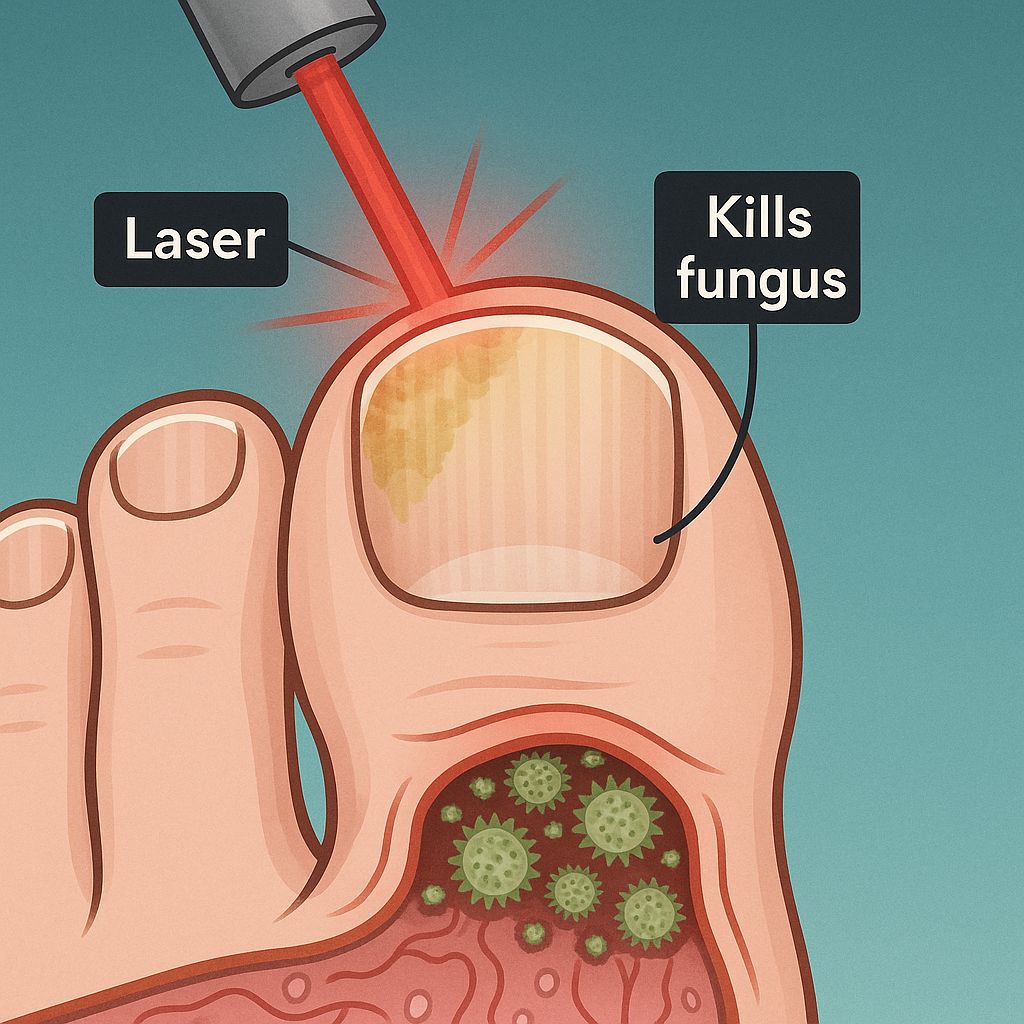
How Laser Treatment Kills Fungus
Laser treatment is so effective because it can target the fungus without damaging the healthy tissue around it. The laser uses a specific wavelength (usually 1064nm Nd:YAG) to heat up the pigments and water molecules in the fungus. This heat damages the cell membrane and denatures the proteins, effectively killing the fungus. Unlike topical treatments, which often can’t penetrate the nail, the laser energy can pass through the keratin structure without any problems. This means it can reach the fungus where it’s hiding without damaging the nail matrix, which is what produces new nail tissue.
How Successful is it Compared to Traditional Methods?
When you compare laser therapy to traditional treatments, you’ll see a big difference in effectiveness. If you take oral antifungals like terbinafine for a full year, you’ll see a clinical cure rate of about 60-70%. But studies show that laser therapy has an improvement rate of 80-90% in a much shorter amount of time. A systematic review in Lasers in Medical Science looked at several clinical trials. It found that people who got Nd:YAG laser treatments had complete cure rates that were almost 30% higher than people who only used topical solutions. Plus, laser therapy gets rid of the problem of people not taking their daily medication, which can cause treatment failures if they miss doses.
Comparative studies that track long-term outcomes provide the most convincing proof. After a year and a half, those who underwent laser therapy showed considerably lower recurrence rates (less than 10%) compared to those who were treated with oral drugs (20-25% recurrence). This indicates that laser treatment is more effective at eliminating the fungal infection, leaving fewer dormant spores that can reactivate the condition in the future.
Treatment Expectations and Post-Treatment
Usually, laser treatment sessions last between 15-30 minutes, depending on how many nails need treatment. The procedure is almost painless, with most patients reporting only a slight warming sensation as the laser passes over the nail. No anesthesia is required, and you can go back to your normal activities right away with no downtime. Most treatment plans require 3-4 sessions spaced 4-6 weeks apart for best results, though this can vary based on how severe the infection is.
After the treatment, the nail will improve according to its natural growth cycle. The first visible signs of a healthier nail usually appear within 3-4 months as the new, uninfected nail grows from the matrix. Complete visual improvement may take 9-12 months – the time it takes for an entirely new toenail to replace the infected one. This timeline highlights why early intervention is so important; treating at the first signs of infection means there is less damaged nail to grow out.
Price Points and Health Insurance
Usually, laser therapy can run from $750 to $1,500 for the entire process. Even though this may seem more expensive than regular medicine, many patients find that the overall cost is similar when you take into account the cost of long-term oral medication and the necessary liver function tests that come with it. Plus, the higher success rates and lower chance of the fungus coming back often make laser treatment more cost-effective over time by avoiding multiple rounds of treatment.
Whether or not your insurance will cover laser treatment for toenail fungus depends on your provider. Medicare and most private insurance companies consider these treatments to be cosmetic, so you’ll have to pay for them yourself. However, some podiatrists offer financing options to make the treatments more affordable. If you have diabetes or a weakened immune system and the fungal infection is a health risk, your doctor may be able to provide documentation of medical necessity to help you get coverage. For more information on treatment options, you can explore this guide to laser nail therapy.
Photodynamic Therapy: Using Light to Destroy Toenail Fungus
Photodynamic therapy (PDT) is a new and exciting treatment that uses light energy and special photosensitizing compounds to kill toenail fungus. The treatment involves two steps. First, a photosensitizing agent is applied to the infected nail. This agent is absorbed by the fungal cells. Then, the nail is exposed to a certain wavelength of light. This light activates the photosensitizing agent, which produces reactive oxygen species. These species destroy the fungal cells from the inside. This treatment is targeted, meaning it only affects the infected cells and leaves the healthy cells alone. This makes it a powerful and effective treatment for toenail fungus.
Research has found that PDT has a success rate of 73-91% in patients who had not responded to standard treatments. This method is particularly useful for patients who cannot take oral antifungals because they have liver problems or are taking other medications that interact with them. Furthermore, PDT, which destroys the fungus through chemical reactions, often requires fewer treatment sessions to completely eliminate the fungus than laser therapy, which primarily uses heat.
Understanding Photosensitizing Agents
Photosensitizers are commonly used in toenail fungus treatments. These include 5-aminolevulinic acid (5-ALA), methyl aminolevulinate (MAL), or newer compounds that are proprietary. These molecules have the ability to penetrate the nail plate and are metabolized by the cells of the fungus into protoporphyrin IX (PpIX). PpIX has a strong absorption of specific light wavelengths. When PpIX, which has accumulated, is exposed to the right light source, it transfers energy to oxygen molecules that are in the tissue. These are then converted into reactive oxygen species, primarily singlet oxygen, that oxidize components of the fungal cell that are vital.
What makes this method so effective is its ability to target the fungus specifically. The fungus cells take in much more of these light-sensitive compounds than human cells do because of differences in how they metabolize substances and their cell walls. This means that when the light activates the compounds, it is the fungus that is primarily damaged, not the human cells.
Latest developments in photosensitizer formulations are now focusing on improving nail penetration using nanoemulsion technology and chemical penetration enhancers. These advancements tackle the main problem in PDT for onychomycosis, which is to ensure that the photosensitizing agent can be delivered adequately through the dense keratin structure of the nail plate to reach the fungus in the nail bed.
What to Expect from the Treatment Procedure and Sessions
Overview of the Photodynamic Therapy Procedure
Session 1: Photosensitizer is applied (60-90 min penetration time) followed by 20 min light exposure
Interim: 1-2 week recovery period
Session 2: Repeat application and light exposure
Interim: 1-2 week recovery period
Session 3: Last application and light exposure
Follow-up: Clinical assessment at 3, 6, and 12 months
Success rate: 80-85% complete cure with proper protocol adherenceA common PDT process involves three treatment sessions that are spaced 1-2 weeks apart. Each session starts with mechanical debridement of the thickened nail to improve penetration, then the photosensitizing agent is applied. The compound requires 60-90 minutes of contact time under occlusion (covered with a light-blocking bandage) to adequately penetrate and accumulate in fungal cells. After this incubation period, the nail is exposed to the appropriate light source—typically red light (630-635nm) or blue light (405-420nm) depending on the specific photosensitizer used—for 10-20 minutes per treatment area.
Success Against Stubborn Strains
Photodynamic therapy offers a distinct advantage over other treatments in that it is highly effective against drug-resistant strains of fungus. Traditional antifungals target specific metabolic pathways, while PDT uses an oxidative damage mechanism to attack multiple cellular structures at once, making it nearly impossible for resistance to develop. Clinical studies have shown that PDT is over 80% effective against strains of Trichophyton rubrum that are completely resistant to terbinafine and itraconazole. This makes PDT an excellent option for patients who have not had success with traditional treatments.
PDT’s ability to target multiple areas at once makes it incredibly versatile against various types of fungus. Some topical treatments may work well against some organisms but not others. However, the oxidative damage caused by PDT is equally damaging to Trichophyton, Candida, and Aspergillus species, which are the three most common causes of onychomycosis. This ability to work against a broad spectrum of organisms means that there is no need to identify the exact pathogen before starting treatment, making the treatment process much more straightforward.
Top 5 Home-Based Light Therapy Devices
As more and more people are seeking convenient treatments that they can do at home, there has been an increase in the production of light therapy devices designed for consumer use. While these devices are not as powerful as the professional equipment you would find in a clinic, they can be used to supplement treatments between clinical sessions or for maintenance therapy after a successful treatment. The most recent devices include advanced safety features and use wavelengths that have been optimized based on clinical research.
1. Lunula Cold Laser System
Primarily used in a clinical setting, the Lunula system is the cream of the crop when it comes to laser technology, using a dual-wavelength approach (637nm and 405nm). This system targets the fungal cells and boosts the body’s immune response all at once, without producing any heat, so there’s no pain during the treatment. Clinical data shows a very impressive 89% improvement rate, with no side effects. While the full system is still only available in a clinic, Lunula now offers a smaller maintenance device for use at home after the professional treatment courses are completed.
2. Cure Ex Nail Fungus Treatment Laser Device
The Cure Ex Nail Fungus Treatment Laser Device is an FDA-approved device that uses a 905nm wavelength laser designed for home use. It is easy to use and only requires 7 minutes of treatment per nail, 4 times a week. Independent tests have shown that it has a 77% improvement rate when used regularly for 4 months. The best results are achieved when it is used in combination with topical treatments. The device has a rechargeable battery that can provide up to 30 treatments per charge, making it perfect for travel.
3. Light Therapy Sock for Nail Fungus
With a unique approach, this cutting-edge system provides red light therapy (630-660nm) through bendable LED panels built into a cozy sock design. This hands-free method enables the simultaneous treatment of several toes during 30-minute sessions while you unwind or work. Even though it requires longer treatment sessions than targeted lasers, the extensive coverage proves especially effective for patients with several infected nails. User studies report 70% satisfaction rates when used daily for 6 months.
4. NailRENEW Laser Device
The NailRENEW laser device is a small, easy-to-use tool that combines a 905nm laser with blue light therapy (470nm) for a two-pronged approach to treatment. The laser penetrates the nail to reach the fungus, while the blue light provides surface-level antimicrobial effects. Each treatment session is quick and easy, taking just 7 minutes per nail. It’s recommended that you use the device 3-4 times a week. The device includes a built-in timer and automatic shut-off to prevent you from overdoing it. Clinical trials have shown that the device is moderately effective, with the best results seen in mild to moderate infections.
5. Zerbace Fungus Removal Gel with Blue Light
This unique system combines a powerful antifungal gel with a blue light activation device. The gel is enhanced with nano-silver particles and tea tree oil, which are delivered through proprietary penetration enhancers. The 405nm blue light activates the photosensitive compounds. This two-pronged approach tackles the issue of medication delivery through the nail and the need to kill the fungus beneath it. While it requires a longer treatment period than professional systems, its affordability makes it a great option for early intervention.
Nanotech-based Toenail Fungus Creams
For years, the biggest hurdle for topical toenail fungus treatments has been getting the medication to the actual fungus, which is located underneath the nail. Nanotechnology has changed everything. It allows us to create tiny delivery vehicles for the medication that can travel through the miniscule channels in the nail’s keratin. These high-tech creams can deliver up to 35 times more medication to the fungus than traditional topicals.
The Role of Nanoparticles in Enhancing Drug Penetration
Nanoparticle technology revolutionizes drug delivery by introducing several groundbreaking methods. Firstly, these minute carriers, usually 10-200 nanometers in diameter, can carry antifungal compounds through the natural pores and cracks in the nail that would typically obstruct larger molecules. Secondly, lipid-based nanocarriers can temporarily integrate with the keratin structure, creating wider channels for drug passage. Lastly, specific nanoparticles can slowly release drugs over a period of time, ensuring that therapeutic concentrations are maintained at the site of the infection for days instead of hours.
Exciting new developments include the use of nanoparticles that are positively charged. These bond to the negatively charged surface of the nail, forming a reservoir for medication that can’t be washed away and is resistant to mechanical forces. This technology greatly improves the ease of treatment by reducing the need for daily applications to just twice a week, while maintaining higher and more consistent levels of medication than can be achieved with daily applications of traditional formulations.
Newest Nano-Enhanced Solutions Approved by the FDA
The new generation of antifungals enhanced by nanotechnology and approved by the FDA mark a significant advancement in the effectiveness of topical treatments. Liposomal terbinafine delivery systems have shown in lab studies to penetrate the nail up to 1000 times more than traditional cream formulations. Clinical trials indicate that almost 65-70% of patients are completely cured with these advanced formulations. This is nearly twice the typical 30-35% achieved with traditional topicals. Also, these formulations have sustained-release properties, reducing the frequency of application to once a day or even three times a week.
The hybrid nanocarrier systems that merge several penetration-enhancing technologies are notably encouraging. The most recent sanctioned formulations blend both water-soluble and lipid-soluble elements in one delivery system, tackling the intricate barrier attributes of the nail plate. These advanced systems adjust to shifting microenvironments as they move from the nail surface to the nail bed, refining drug release exactly where it’s required. For more information on nail treatments, check out this guide on laser nail therapy.
Pairing Nanotechnology with Other Methods
Nowadays, the most successful treatment plans pair nanotechnology-enhanced creams with physical or energy-based treatments. Pre-treating nails with controlled microneedling devices creates temporary microchannels that significantly improve nanoparticle penetration. Research has shown that this combined method increases medication delivery by up to 80% compared to only using nano-formulations. In the same way, applying nano-enhanced medications right after laser treatment sessions capitalizes on the temporary permeability increase from thermal effects.
If you have a stubborn or severe infection, you may want to consider a triple-therapy protocol that combines laser treatment, microneedling, and nano-enhanced medications. These treatments have shown to be incredibly effective, with success rates nearing 95% in published case studies. Though these treatments are more intensive and costly, they offer a glimmer of hope for patients who have tried and failed to treat their infection with traditional methods.
Intelligent Fungal Treatment Monitoring Systems
Recent advancements in fungal treatment include smart monitoring technologies that follow the progress of the treatment and the environmental conditions. These systems offer objective information on nail improvement, adherence to medication application, and risk factors—turning the traditionally subjective evaluation process into a precise science.
Sweat-Monitoring Insoles
Excessive moisture is a breeding ground for fungus, and new insole technology can monitor the sweat levels in your feet throughout the day. These thin, comfortable sensors fit inside regular shoes and connect wirelessly to apps on your phone that will alert you when the moisture levels in your shoes reach a level that is conducive to fungus growth. Some advanced models can even track temperature changes and can recommend when to apply powder or change your socks based on your personal sweat patterns. For patients who have recurring infections, these systems can help identify which activities or shoes are associated with problematic moisture levels. If you’re looking for effective treatments, learn about what kills toenail fungus instantly.
Apps and Devices for Treatment Consistency
One of the biggest hurdles in treating toenail fungus is ensuring consistent application of medication. Studies have shown that skipping applications directly leads to treatment failure. New technology in the form of smart bottle caps for topical medications can help. These caps record each time the bottle is opened, creating an accurate record of applications that can be synced to treatment monitoring apps. These apps can send reminders based on the specific treatment protocol prescribed and generate progress reports that can be shared directly with doctors. Some of the more advanced systems even incorporate image recognition technology that can evaluate application technique through brief video recordings, ensuring that medication is applied correctly.
The most advanced systems combine data on medication adherence with photo monitoring of nails to create a complete treatment dashboard. These systems use standardised imaging to objectively track changes in the clarity, thickness, and discolouration of the nail – measurements that are strongly linked to a mycological cure but hard to assess with the naked eye. This objective data helps keep patients motivated during the long treatment process by documenting subtle improvements that might otherwise be missed.
Choosing the Right Treatment: How to Navigate Your Options
Choosing the right treatment for toenail fungus can be tricky. You need to consider the severity of the infection, your overall health, and what treatments are available to you. Fortunately, new diagnostic tools can help doctors pinpoint the best treatment for you, instead of using the old method of trial and error, which can be time-consuming and frustrating.
Technological Innovations in Diagnosing Toenail Fungus
Advanced diagnostic tools have transformed the way we identify fungi, replacing the subjective visual assessment with a precise characterization of the pathogen. Polymerase chain reaction (PCR) testing now allows for same-day identification of fungi with 99% accuracy, compared to traditional cultures that take weeks and often result in false negatives. This rapid identification allows for the selection of treatment specifically matched to the susceptibility patterns of the identified organism. Additionally, the new confocal laser scanning microscopy allows for non-invasive imaging of living fungal elements under the nail plate, confirming active infection without the need for painful nail sampling.
One of the most useful tools for planning treatment is optical coherence tomography (OCT), which can measure the exact thickness and density of the nail plate. These measurements can help predict which treatment will work best. For example, nails that are thicker than 3mm usually do not respond well to topical treatments, no matter what kind they are. Nails with a lot of horizontal ridging often need a combination of treatments because the medication does not penetrate evenly. By using these measurements, doctors can avoid wasting time with treatments that will not work.
How Bad is It?
Doctors have found a new way to measure how severe a toenail fungus infection is, and it’s incredibly accurate. They use a standard tool called the Onychomycosis Severity Index (OSI) along with a digital image of the infected nail. The image helps them calculate exactly what percentage of the nail is infected, and they get the same answer 98% of the time. This is really important because the more of the nail that’s infected, the harder the infection is to treat. Doctors use this information to decide how to treat the infection. If less than 30% of the nail is infected, they usually use a topical treatment that’s been improved with nanotechnology. If more than 60% of the nail is infected, they usually need to use a treatment like a laser or photodynamic therapy (PDT). If the infection is somewhere in the middle, they look at other factors like whether the infection is in the nail matrix (the part of the nail that’s under the skin) and how long the nail has been infected to decide what treatment to use.
Aside from a simple visual check, new biochemical severity markers can measure keratin degradation compounds in nail samples to accurately predict the severity of an infection. These biomarkers can identify infections that are rapidly progressing and would benefit from immediate, intensive treatment versus infections that are more slow-moving where conservative treatments would be appropriate. This personalized risk stratification prevents both the undertreatment of aggressive infections and the overtreatment of slowly progressing cases.
When to Use Multiple Technologies Together
Combining therapies can offer increased benefits, but it also adds complexity and cost. Studies have shown that patients who have three or more risk factors—diabetes, previous unsuccessful treatments, more than 50% nail involvement, symptoms for more than 5 years, or matrix involvement—see a 40% higher cure rate with combined approaches compared to a single therapy. The most effective combinations usually involve an energy-based treatment (like a laser or PDT) with nano-enhanced topicals, creating a powerful one-two punch of destroying the fungus and then delivering medication over a sustained period. For severe cases, adding a mechanical intervention like controlled micro-drilling or nail avulsion before other treatments can significantly improve the results by getting rid of dense keratin barriers.
Comparing Costs and Benefits of Different Treatments
Advanced treatments often have a higher upfront cost, but a complete cost analysis should also take into account the length of treatment, the likelihood of success, recurrence rates, and the impact on quality of life. Nano-enhanced topicals have the lowest initial cost ($150-$300 for a full treatment course), but they require a longer treatment period (9-12 months) and have moderate success rates (65-70%). Laser therapy has a higher initial cost ($800-$1,500), but it offers a shorter treatment period (3-4 sessions over 3 months) and significantly higher success rates (85-90%). For patients who have tried traditional treatments without success, the higher initial cost of advanced treatments often ends up being more cost-effective in the long run because it avoids the need for multiple unsuccessful treatment cycles.
The Tech-Savvy Prevention Plan
The best way to tackle toenail fungus is to combine advanced treatments with a well-rounded prevention plan. Gone are the days of only relying on basic hygiene to prevent fungal infections. Today, we have access to high-tech tools that help stop fungus in its tracks and make it hard for it to come back. For patients who have successfully gotten rid of their toenail fungus, these tech-savvy prevention tools can help keep it from coming back. In fact, while historically the recurrence rate of toenail fungus was 50% within two years, today that rate is under 15% when modern prevention tools are used consistently.
Modern Antifungal Footwear
Goodbye traditional cotton socks, hello advanced moisture-wicking fabrics! These modern fabrics are laced with nanoparticles of copper, silver, or zinc oxide that destroy fungus on contact. They can withstand hundreds of washes while maintaining their antimicrobial properties and can reduce fungal loads by up to 99.9% compared to untreated fabrics. Similarly, the latest shoe insoles are made with materials that slowly release antimicrobial compounds, providing protection for 3-6 months of daily use. Athletes and others who are at high risk can benefit from specialized socks with individual toe compartments that prevent the spread of fungus from one toe to another and reduce moisture buildup in the spaces between the toes where infections often start.
UV Sterilization for Shoes and Socks
Ultraviolet sterilization devices created specifically for shoes offer a level of disinfection that traditional cleaning methods can’t match. These systems usually use UVC light (wavelengths of 100-280nm) to destroy the DNA of fungi, preventing them from reproducing even if some spores survive. Some of the more advanced models also generate ozone, which can penetrate into the material of the shoe where light can’t reach. Clinical tests have shown that these devices can reduce the amount of fungus by over 99.7% with just a 15-minute treatment cycle, effectively getting rid of any leftover fungal elements that could cause a reinfection. For the best protection, it’s recommended to sanitize your shoes daily, especially if they’re athletic shoes that see a lot of sweat.
Intelligent Humidity Sensors
Regulating your environment is a key preventative measure, as fungi flourish in damp conditions. Newly developed wireless humidity monitors are designed to be used in closets and shoe storage areas. They constantly track conditions and alert users when the humidity levels rise above 60%—the point at which fungi growth rapidly increases. More sophisticated systems can be integrated with smart home technology to automatically switch on dehumidifiers or circulate air when conditions become problematic. These systems are useful for those living in tropical climates or for those who face challenges with seasonal humidity. They help to maintain a shoe storage environment that prevents fungi from multiplying between uses. For more solutions, check out these instant toenail fungus home remedies.
By bringing together these preventative measures, we can create a multi-layered shield that tackles the infection process from start to finish. This combination of active anti-fungal materials, environmental control, and regular disinfection can even help those genetically predisposed to fungal infections reduce their risk significantly. Following a successful treatment, prevention protocols tailored to the individual’s risk profile are now the norm.
Revolutionary Fungal Treatment Is Now Available
The world of toenail fungus treatment has changed significantly, providing new hope for those who have been battling with this stubborn condition. The latest technological methods tackle the main issues that have traditionally made these infections so hard to get rid of—getting through the nail barrier, keeping consistent medication levels, and stopping reinfection. For patients who have experienced the disappointment of unsuccessful treatments, these advanced options are not just minor enhancements but game-changing solutions.
Thanks to the combination of diagnostic accuracy and targeted treatments, we can now expect much better results. The old “try it and see” method, which often led to disappointment, has been replaced by modern techniques that provide predictable outcomes based on objective evaluation and personalised treatment choices. This shift from guesswork to science is a welcome change for a condition that has long been plagued by uncertainty in treatment.
What’s most significant about these technologies is that they have completely changed the patient experience. It’s gone from a situation of embarrassment and resignation to one of empowerment and resolution. By blending professional treatments with home management systems, individuals are taking active roles in their recovery. They are no longer just passive recipients of care. The psychological benefits of this shift – regaining confidence in appearance and reducing anxiety about infection spread – go far beyond the physical improvement of the nails themselves.
Comparison of Success Rates for Different Treatments
Topical Solutions (Traditional): 15-30%
Antifungals (Oral): 60-70%
Topicals (Nano-Enhanced): 65-75%
Therapy (Photodynamic): 75-85%
Treatment (Laser): 85-90%
Approaches (Combination): 90-95%Commonly Asked Questions
People who are thinking about getting advanced treatments usually have a lot of questions about these high-tech options. The answers below cover the most frequent worries and help create a clear picture of what to expect from the treatment results.
What is the duration of laser treatment for curing toenail fungus?
Usually, laser treatment involves 3-4 sessions that are spaced 4-6 weeks apart. Each session lasts for about 15-30 minutes. The fungus is effectively killed during these sessions, but visible nail improvement follows the natural growth cycle. Most patients observe clear improvement within 3-4 months when the new, uninfected nail starts growing from the base. For more information on effective treatments, you can refer to this laser nail therapy guide. Complete visual transformation typically takes 9-12 months—the time required for the entire nail to regrow. This timeline can vary based on individual nail growth rates. Younger patients usually see faster results than older adults.
Do advanced toenail fungus treatments hurt?
Not at all. The latest treatments use technology to ensure you feel as little discomfort as possible. Laser therapy, for example, feels like a gentle warming sensation. Photodynamic therapy doesn’t cause any sensation when the light is applied, although you might feel a little sensitive for a day or two afterwards. If you’re having microneedling to help the treatment penetrate your toenail, you’ll have a numbing cream applied first to make sure it doesn’t hurt. Plus, these treatments don’t have the side effects that you can get with oral antifungal medicines, so they’re a safe and comfortable way to get rid of toenail fungus.
How do the results of new technologies compare to those of traditional treatments?
Advanced technological treatments are far more successful than traditional methods. Traditional topicals only have a complete cure rate of 15-30%, while laser therapy and photodynamic therapy have a success rate of 85-90% in clinical studies. Not only is this a huge improvement, but these treatments also take less time and have fewer side effects. What’s even more impressive is that these advanced options work on fungal infections that have failed multiple traditional treatments. For patients with long-term or resistant infections, technological treatments are about three times more likely to completely get rid of the infection than traditional treatments.
Can I use several advanced treatments at the same time?
Not only is it possible to use a combination of treatments, but it is often recommended for the best results. Many medical professionals are now using complementary treatment methods that combine energy-based treatments (such as laser or photodynamic therapy) with topical applications that have been enhanced with nano-technology. The energy treatments quickly reduce the amount of fungus, while also temporarily increasing the permeability of the nail, which allows the medication to penetrate more effectively. This combined effect can result in success rates of up to 95% when the right combination of treatments is chosen. However, it is important to have these combinations professionally directed, as some combinations can cause unnecessary irritation or be less effective if they are not used in the right order.
Does insurance cover advanced treatments for toenail fungus?
Insurance coverage for advanced toenail fungus treatments can vary greatly depending on the provider and the policy. Most insurance companies currently consider laser and photodynamic therapies to be cosmetic procedures, not medical necessities, which can limit coverage. However, as more evidence shows the health risks of untreated toenail fungus, especially for people with diabetes, this is slowly changing. Some insurance plans now cover part of the cost if there is a documented medical need, such as pain, limited function, or risk of a secondary infection. Many treatment centers offer financing options, and the cost-effectiveness often becomes clear when you compare the total cost of repeated traditional treatments that don’t work with the higher success rates of advanced treatments.
Dealing with toenail fungus doesn’t mean you have to put up with treatments that don’t work or strong drugs that have worrying side effects. The technology of today offers treatments that are incredibly effective and very safe. If you’re someone who suffers from recurring fungal infections, these advanced treatments offer real hope for a total cure and a return to healthy, clear nails.
If you’re keen to find out how cutting-edge tech treatments can get rid of your toenail fungus, Certified Foot clinics provide a thorough evaluation and a personalized treatment plan using the newest FDA-approved options.