Key Takeaways
- Several effective alternatives to surgery exist for fungal toenails, including oral medications, topical solutions, and laser therapy that can effectively treat infections without surgical intervention.
- Essential oils like tea tree, oregano, and thyme have shown promising antifungal properties when used consistently as part of a comprehensive treatment approach.
- Nail debridement performed by a podiatrist can significantly improve the effectiveness of other treatments by reducing the fungal load in the affected nail.
- Surgery should only be considered when conservative treatments have failed, the infection is severe, or pain significantly impacts daily activities.
- Prevention strategies including proper foot hygiene, appropriate footwear, and early intervention are crucial for avoiding both initial infections and recurrence after treatment.
That yellowing, thickened toenail isn’t just an unsightly cosmetic issue—it could be signaling a fungal infection that requires attention. While surgical removal might seem like a definitive solution, there are numerous effective alternatives worth exploring before taking that step. The team at Natural Foot Solutions specializes in helping patients navigate the full spectrum of treatment options, prioritizing non-invasive approaches whenever possible.
Why You Shouldn’t Ignore That Yellow Toenail
Fungal toenail infections (onychomycosis) affect approximately 10% of the general population, with prevalence increasing to nearly 50% in those over 70 years old. What begins as a small white or yellow spot can gradually spread, causing the entire nail to become discolored, thickened, and brittle. Left untreated, these infections can worsen, causing pain, difficulty walking, and potentially spreading to other nails or even to other people.
Beyond the physical discomfort, untreated fungal infections can significantly impact quality of life. Many patients report embarrassment about the appearance of their feet, leading them to avoid activities like swimming or wearing open-toed shoes. The psychological burden shouldn’t be underestimated, especially when simple interventions could resolve the issue.
Most importantly, ignoring fungal infections can be particularly dangerous for individuals with diabetes or compromised immune systems, where even minor foot problems can escalate into serious complications. Early intervention not only improves treatment outcomes but can prevent the need for more invasive procedures down the line.
5 Effective Alternatives to Fungal Toenail Surgery
Before considering surgical intervention, numerous evidence-based alternatives exist that can effectively eliminate fungal infections while preserving the natural nail. These options range from prescription medications to professional treatments and natural remedies, often achieving excellent results when used appropriately and consistently.
Oral Antifungal Medications
Prescription oral antifungals like terbinafine (Lamisil) and itraconazole (Sporanox) work from within to target the infection at its source. These medications typically require a 6-12 week course of treatment and work by helping a new, healthy nail grow free of infection, gradually replacing the infected portion. Success rates can reach 70-80% for complete cures, making them one of the most effective non-surgical interventions available.
The primary advantage of oral medications is their ability to reach the nail bed through the bloodstream, addressing deep-seated infections that topical treatments might miss. However, they do require monitoring with periodic liver function tests and may interact with other medications, making them unsuitable for some patients with existing health conditions. For those seeking effective alternatives, here are some effective approaches for toenail fungus treatment.
Prescription-Strength Topical Solutions
Medically-formulated topical solutions provide a targeted approach without systemic effects. Products like ciclopirox (Penlac) nail lacquer and tavaborole (Kerydin) are applied directly to the affected nails, typically once daily for up to 48 weeks. While requiring patience and consistent application, these solutions can effectively treat mild to moderate infections, especially when combined with regular nail debridement. For those dealing with severe or mild toenail fungus, these topical treatments offer a promising alternative.
Newer topical formulations have significantly improved penetration compared to older products, allowing the active ingredients to better reach the nail bed where the fungus resides. The main benefits include minimal side effects and compatibility with most other medications, though treatment time is considerably longer than with oral options.
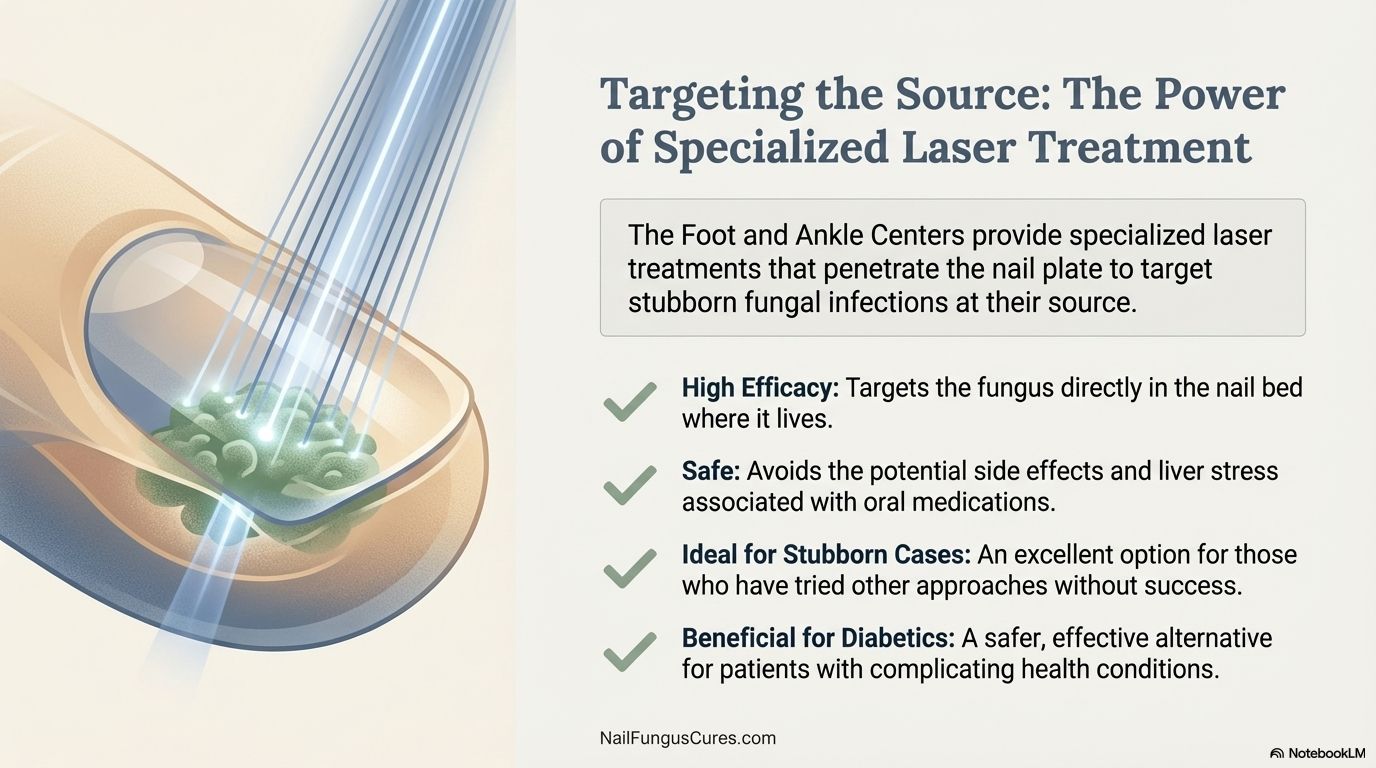
Laser Therapy Treatment
Laser therapy represents one of the most innovative non-surgical approaches to treating fungal nails. This technology uses specific wavelengths of light to target and destroy fungal organisms without damaging the surrounding tissue. Most patients require 3-4 sessions spaced several weeks apart, with noticeable improvement often visible after the first few treatments.
The procedure itself is virtually painless, requiring no anesthesia and allowing patients to resume normal activities immediately afterward. Research shows success rates between 60-80% for appropriate candidates, with the added advantage of no drug interactions or systemic side effects. While typically more expensive than medication-based approaches and not always covered by insurance, many patients find the convenience and effectiveness well worth the investment.
Natural Essential Oil Remedies
Essential oils have garnered significant attention for their natural antifungal properties. Tea tree oil (Melaleuca alternifolia) stands out as one of the most studied options, with research demonstrating its ability to penetrate the nail plate and combat fungal pathogens. Other powerful options include oregano oil, which contains carvacrol and thymol, compounds with documented antifungal efficacy, and thyme oil, which has shown promising results against dermatophytes responsible for nail infections.
For maximum effectiveness, these oils should be applied consistently to clean, dry nails at least twice daily, often diluted in a carrier oil like coconut or olive oil to prevent skin irritation. While results typically take longer to appear compared to prescription options, many patients appreciate the minimal side effects and holistic approach. The most successful protocols often combine multiple oils and include gentle filing of the nail surface to improve penetration.
Nail Debridement by a Podiatrist
Professional debridement involves the careful removal of infected nail material by a trained podiatrist. This procedure significantly reduces the fungal load in the nail and creates a smoother surface that enhances the effectiveness of topical treatments. Using specialized instruments, the podiatrist thins the nail and removes debris from underneath, often providing immediate relief from pressure and discomfort while facilitating the penetration of antifungal agents.
Most patients require periodic debridement sessions, typically every 6-8 weeks throughout the treatment course. This approach is particularly beneficial for elderly patients and those with diabetes who should avoid self-trimming due to risk of injury. When combined with appropriate antifungal therapy, debridement can dramatically improve outcomes while preserving the natural nail structure.
When Surgery Becomes Necessary for Fungal Toenails
While non-surgical approaches resolve most fungal infections, certain circumstances may warrant surgical intervention. Understanding these scenarios helps patients make informed decisions about their treatment progression. Surgery is typically considered only after conservative measures have been exhausted or when specific clinical indications present themselves.
Signs Your Infection Requires Surgical Intervention
Several key indicators suggest that surgery might be the most appropriate course of action. Persistent infections that show no improvement after 6-12 months of consistent treatment with other modalities often benefit from a surgical approach. Additionally, severe pain that impacts daily activities, especially if caused by pressure from significantly thickened nails, may necessitate removal to provide relief.
Recurrent infections despite appropriate preventive measures represent another common indication for surgical management. Some patients experience anatomical factors that predispose them to repeated infections, such as severely deformed nails or chronic ingrowth patterns that create environments favorable to fungal growth. In patients with diabetes or peripheral vascular disease, advanced infections that pose risks for complications may require prompt surgical attention to prevent more serious consequences. For more information on surgical options, you can read about surgical nail removal for fungal infections.
What to Expect During a Consultation
A comprehensive surgical consultation begins with a thorough examination of the affected nails and surrounding tissues. The podiatrist will assess the extent of the infection, evaluate nail thickness and deformity, and check circulation to ensure adequate healing potential. Medical history review is essential, with particular attention to conditions like diabetes, immunosuppression, or peripheral vascular disease that might influence surgical decisions or recovery. For those exploring alternatives, understanding effective approaches to toenail fungus treatment can be beneficial.
Diagnostic testing may include nail clippings for fungal culture or PCR testing to confirm the specific pathogen involved. The doctor will discuss your treatment history, documenting previous approaches and their effectiveness. Based on this complete assessment, they’ll present appropriate surgical options, clearly explaining the benefits, risks, and expected recovery timeline for each procedure. This collaborative decision-making process ensures the selected approach aligns with both clinical needs and patient preferences.
Types of Fungal Toenail Removal Procedures
Surgical management of fungal toenails encompasses several distinct procedures, each tailored to specific clinical presentations. The appropriate approach depends on factors including infection severity, nail deformity, pain level, and likelihood of recurrence. For a detailed overview of these procedures, you can explore more about surgical nail removal for fungal nail infections. Understanding these options helps patients participate meaningfully in treatment decisions.
Partial Nail Avulsion: The Targeted Approach
Partial nail avulsion involves surgically removing only the infected portion of the nail while preserving healthy tissue. This technique is particularly valuable when infection affects just one section of the nail or extends to the nail bed beneath. After administering local anesthesia, the podiatrist carefully separates the diseased nail portion from the underlying bed and removes it, often applying topical antifungal medication directly to the exposed area.
Recovery from partial avulsion typically proceeds more quickly than with complete removal, with most patients returning to regular footwear within 1-2 weeks. This approach maintains nail appearance and function while effectively addressing the infection. For optimal results, patients should continue prescribed topical treatments to the exposed nail bed until the new nail grows in completely.
Complete Nail Removal: When It’s Recommended
Complete nail removal (total avulsion) becomes necessary when infection extends throughout the entire nail or when severe deformity is present. This procedure removes the entire nail plate from its attachment to the underlying nail bed, eliminating all infected tissue in one definitive intervention.
Patient Experience: Complete Nail Removal
“I had struggled with a thick, painful toenail for years, trying countless treatments without success. After discussing options with my podiatrist, I opted for complete removal. The procedure itself was quick—about 15 minutes under local anesthesia. Recovery required about two weeks of limited activity, but the relief was immediate. Six months later, my nail is growing back healthier than it’s been in years.”
— Maria T., 58
The procedure begins with thorough cleaning and local anesthesia to ensure comfort. Using specialized instruments, the podiatrist carefully separates the nail from surrounding tissues and removes it entirely. Afterward, an antifungal agent is typically applied directly to the exposed nail bed. A sterile dressing protects the area, and patients receive detailed aftercare instructions.
While recovery requires more careful attention than partial removal, most patients experience significant pain relief almost immediately following the procedure. Daily activities can usually resume within 2-3 days, though protective footwear is recommended for approximately 2-3 weeks. The nail typically begins to regrow within 3-4 months, though complete regrowth takes 12-18 months.
Follow-up appointments are essential to monitor healing and ensure the new nail grows in properly without recurrent infection. Some patients choose to maintain the nail-free state with periodic debridement if they’ve experienced severe, recurrent infections in the past.
Matrixectomy: Preventing Nail Regrowth
For patients with severe recurrent infections or significant nail deformity, matrixectomy provides a permanent solution by removing not only the nail but also the nail matrix (growth center). This procedure prevents the nail from growing back, eliminating the possibility of future infections in that nail. It’s typically performed using either chemical agents like phenol or sodium hydroxide, or surgical excision of the matrix tissue, depending on the specific clinical situation and patient factors.
Step-by-Step Recovery After Toenail Surgery
Proper post-surgical care significantly influences both healing time and outcomes after toenail removal procedures. Following your podiatrist’s specific instructions is critical, but understanding the general recovery timeline helps patients set realistic expectations and recognize normal healing milestones.
First 48 Hours: Critical Care Period
The immediate post-surgical period requires the most attentive care to minimize complications and establish optimal healing conditions. Keep the surgical site elevated above heart level whenever possible for the first 24-48 hours to reduce swelling and throbbing. Ice application (20 minutes on, 20 minutes off) helps manage both inflammation and discomfort, particularly during the first day. Maintain the original dressing intact and dry until your first follow-up appointment, typically scheduled 1-2 days after surgery. For those dealing with persistent issues, exploring professional therapy for stubborn nail fungus might be beneficial.
Pain management typically involves prescribed or over-the-counter medications according to your doctor’s recommendations. Most patients report that pain peaks 8-12 hours after the procedure as the local anesthetic wears off, then gradually subsides. Limiting weight-bearing activities and using surgical shoes or open-toed footwear prevents pressure on the healing site. Watch for signs of infection including increased pain, redness extending beyond the toe, warmth, or discharge with odor—contacting your provider immediately if these develop.
1-2 Weeks: Wound Healing Phase
As initial healing progresses, your podiatrist will likely change your dressing and provide specific cleaning instructions. Typically, gentle daily cleaning with mild soap and water begins at this stage, followed by application of prescribed topical medications and fresh, sterile dressings. Avoid soaking the area completely until given explicit permission, as prolonged moisture can compromise healing tissues.
Most patients can gradually resume light activities during this period, though high-impact exercise, swimming, and excessive walking should still be avoided. Appropriate footwear remains essential, with most podiatrists recommending open-toed surgical shoes or sandals that prevent pressure on the healing nail bed. Continue monitoring for signs of infection and attend all scheduled follow-up appointments, which allow your provider to assess healing progress and address any concerns.
3-6 Weeks: Getting Back to Normal Activities
By the 3-6 week mark, most patients have achieved sufficient healing to resume normal activities, though individual recovery timelines vary based on the specific procedure, overall health, and adherence to post-operative instructions. The surgical site typically appears pink but should no longer be actively draining or significantly painful. Most patients can transition to regular closed-toe shoes, though particularly snug footwear might still cause discomfort. For those dealing with severe toenail fungus, additional care might be necessary to ensure complete recovery.
This period marks an important transition from wound care to preventative measures against recurrence. Your podiatrist may recommend beginning specific antifungal treatments to the nail bed and surrounding skin to prevent reinfection as the new nail begins to emerge. Maintaining excellent hygiene practices becomes particularly important as activity levels increase and exposure to potential fungal reservoirs resumes.
6-18 Months: Complete Nail Regrowth Timeline
Toenail regrowth represents the longest phase of the recovery process, requiring patience and continued preventative care. Initial nail growth typically becomes visible within 6-8 weeks after surgery, appearing as a thin, somewhat irregular edge at the base of the nail bed. Complete regrowth of a healthy toenail takes between 12-18 months for most adults, with growth proceeding at approximately 1mm per month.
The new nail may initially appear somewhat different in texture or thickness compared to your other toenails, gradually improving in appearance as growth continues. Regular application of recommended antifungal products throughout this period significantly reduces reinfection risk. Periodic assessment by your podiatrist during the regrowth phase ensures that the new nail develops properly without recurrent infection or structural abnormalities.
7 Daily Habits That Prevent Fungal Toenail Recurrence
Successfully treating fungal toenail infections requires not only addressing the current infection but implementing preventative measures to avoid recurrence. Studies show that without proper preventative care, recurrence rates can reach 10-50% within one year of successful treatment. Incorporating these evidence-based practices into your daily routine significantly reduces reinfection risk.
1. Proper Foot Hygiene Routine
Maintaining impeccable foot hygiene forms the foundation of effective prevention. Wash feet daily with mild soap, paying special attention to the spaces between toes where moisture accumulates. Pat feet completely dry rather than rubbing, which can cause micro-abrasions that provide entry points for fungal organisms. Complete drying is crucial, as fungi thrive in warm, moist environments—consider using a hair dryer on a cool setting to thoroughly dry between toes and around nail beds. For additional methods, you might explore treatment methods for athlete’s foot.
Apply antifungal powder or spray as recommended by your podiatrist, especially before putting on socks and shoes. For those with excessive perspiration, aluminum chloride solutions applied to clean, dry feet in the evening can help reduce sweat production. Change socks at midday if feet become notably damp during work or activities, as prolonged moisture significantly increases reinfection risk.
2. Footwear Selection and Care
Shoes create microenvironments that can either promote or inhibit fungal growth, making appropriate selection and maintenance critical to prevention. Choose breathable materials like leather, mesh, or canvas that allow moisture evaporation rather than trapping it against the skin. Ensure adequate toe box width to prevent crowding, which increases perspiration and creates pressure points that may damage nails and surrounding tissues. For those dealing with severe or mild toenail fungus, selecting the right footwear is even more crucial to prevent further complications.
Rotate between at least two pairs of shoes, allowing each pair a minimum 24-hour drying period between wearings. Using shoe dryers or inserting silica gel packets into shoes overnight accelerates moisture removal. Disinfect shoes regularly with UV shoe sanitizers or antifungal sprays formulated specifically for footwear, addressing potential fungal reservoirs that could cause reinfection.
3. Moisture Control Techniques
Managing moisture represents one of the most effective ways to create an environment hostile to fungal proliferation. Moisture-wicking socks made from synthetic blends or specialized fabrics like copper-infused fibers draw perspiration away from the skin surface, significantly reducing the damp conditions fungi require. Consider changing socks midday if you notice dampness, particularly during hot weather or following physical activity. For more insights on effective approaches, check out this article on toenail fungus treatment.
For individuals with hyperhidrosis (excessive sweating), prescription-strength antiperspirants containing aluminum chloride hexahydrate can be applied to clean, dry feet before bed, then washed off in the morning. More advanced cases might benefit from iontophoresis treatments, which use mild electrical currents to temporarily block sweat glands, or in severe cases, botulinum toxin injections to reduce sweat production for several months.
4. Avoiding High-Risk Environments
Certain environments harbor significantly higher concentrations of fungal organisms, increasing exposure risk. Public swimming pools, locker rooms, communal showers, and spa facilities top the list of high-risk locations due to warm, moist conditions and high foot traffic. When visiting these areas, wear protective water shoes or flip-flops at all times to minimize direct contact with potentially contaminated surfaces. Position personal items on clean, dry surfaces rather than directly on floors, and avoid sitting on benches while barefoot. For more on maintaining nail health, check out these tips on restoring nail health after fungal infections.
Home environments can also present risks, particularly bathrooms and areas around swimming pools. Clean shower floors regularly with antifungal cleaners, and consider using antifungal bath mats that can be machine washed weekly. In households where someone has a fungal infection, disinfect bathtubs and shower floors after each use to prevent transmission to other family members.
5. Regular Nail Inspection and Maintenance
Routine nail assessment allows for early identification of potential problems before they progress to established infections. Set a regular schedule—perhaps monthly—to carefully examine your toenails for any changes in color, texture, or thickness. Use good lighting and a magnifying glass if necessary, paying special attention to the edges and corners where infections often begin. Photograph concerning areas to track changes over time, enabling you to detect subtle progression that might otherwise go unnoticed.
Proper trimming techniques significantly reduce infection risk by preventing nail damage that creates entry points for fungi. Cut nails straight across rather than curved, maintaining a length just at or slightly beyond the toe tip. Use dedicated toenail clippers and disinfect them between uses with alcohol or hydrogen peroxide. For thickened nails, professional debridement by a podiatrist helps maintain appropriate thickness and shape, reducing pressure points and potential separation from the nail bed.
Filing plays an important role in prevention by smoothing rough edges that might catch and tear. Always file in a single direction rather than using a sawing motion, which can create nail damage. Consider professional attention for any nails showing signs of trauma, as damaged nails are significantly more susceptible to fungal invasion.
- Inspect nails after activities with higher risk of trauma, such as hiking or intense exercise
- Keep nails clean, dry, and at an appropriate length (not too short or too long)
- Never share nail tools with others, even family members
- Consider periodic professional maintenance every 2-3 months
- Address any nail changes promptly rather than waiting for obvious infection signs
6. Strengthening Your Immune System
Your body’s natural defenses play a crucial role in preventing fungal colonization, making immune system support an essential component of comprehensive prevention. Nutritional factors significantly influence immune function, with adequate protein intake supporting antibody production and immune cell development. Ensure sufficient levels of immune-boosting nutrients including vitamin C, vitamin D, zinc, and selenium through diet or targeted supplementation as recommended by your healthcare provider. Probiotic-rich foods like yogurt, kefir, and fermented vegetables support the gut microbiome, which research increasingly links to overall immune competence.
Lifestyle factors equally impact immune function, with regular moderate exercise enhancing immune surveillance while excessive training can temporarily suppress immunity. Prioritize quality sleep of 7-9 hours nightly, as sleep deprivation notably impairs immune response. Stress management techniques including meditation, deep breathing exercises, or yoga help regulate cortisol levels, preventing the immune suppression associated with chronic stress. For individuals with conditions affecting immune function, such as diabetes or autoimmune disorders, maintaining optimal control of these conditions through appropriate medical management represents a critical aspect of fungal prevention.
7. When to Seek Professional Help
Even with diligent preventative measures, early intervention at the first sign of potential reinfection dramatically improves treatment outcomes and minimizes complications. Contact your podiatrist promptly if you notice nail discoloration (particularly yellow, white, or brown spots), increasing thickness or brittleness, separation of the nail from the bed, or any pain or discomfort associated with the nail. For individuals with risk factors including diabetes, peripheral vascular disease, or immunosuppression, more frequent professional monitoring is recommended, typically every 2-3 months, regardless of symptom presence. For those seeking more information on effective treatments, explore prescription treatments for toenail fungus.
The Final Word on Fungal Toenail Treatment
When dealing with fungal toenail infections, a balanced approach combining appropriate medical interventions with consistent preventative measures yields the best long-term results. While surgery remains a valuable option for severe or resistant cases, the numerous effective alternatives discussed provide viable solutions for many patients. The key to success lies not in finding a single “miracle cure” but in developing a comprehensive treatment plan tailored to your specific clinical presentation and lifestyle factors. Working collaboratively with Natural Foot Solutions ensures you’ll receive guidance based on both clinical expertise and the latest research, helping you achieve not just temporary improvement but lasting nail health.
Frequently Asked Questions
Patients considering treatment for fungal toenail infections typically have numerous questions about their options, expected outcomes, and recovery processes. The following responses address the most common inquiries we receive in our practice, providing evidence-based information to help guide your decision-making process.
Remember that while these answers provide general guidance, individual cases vary significantly based on infection severity, overall health status, and specific nail characteristics. Consultation with a qualified podiatrist remains essential for personalized recommendations tailored to your unique situation.
How can I tell if I have a fungal toenail infection or just a bruised nail?
Distinguishing between fungal infections and traumatic nail injuries can be challenging, as both may cause discoloration and structural changes. Fungal infections typically begin at the tip or side of the nail with yellow or white discoloration that gradually spreads toward the base. The nail often becomes thickened, brittle, and may develop a crumbly texture, particularly along the edges. In contrast, bruised nails (subungual hematomas) appear as reddish-purple or dark areas that don’t spread but grow out with the nail, gradually moving from the base toward the tip. Definitive diagnosis requires professional evaluation, often including microscopic examination of nail clippings or fungal cultures to identify the specific pathogen.
Will my insurance cover fungal toenail treatments or surgery?
Insurance coverage for fungal toenail treatments varies significantly between providers and specific plans. Most insurance companies require documentation of medical necessity rather than covering treatment for purely cosmetic concerns. This typically includes evidence of pain, difficulty with activities, secondary infection, or risk factors like diabetes that elevate the clinical significance of the infection. Prescription medications often receive partial coverage, though laser treatments typically remain uncovered by most plans. Surgical interventions generally receive better coverage when properly documented as medically necessary, but always verify specific benefits with your insurance provider and request pre-authorization when possible.
Can I treat my fungal toenail at home without any medical intervention?
Home remedies may prove effective for very mild or early fungal nail infections, though success rates fall significantly below medical interventions. The most promising home approaches include consistent application of tea tree oil, white vinegar soaks (one part vinegar to two parts water for 15-20 minutes daily), or over-the-counter antifungal preparations containing undecylenic acid. Maintaining impeccable nail hygiene, including regular trimming, filing, and thorough drying, supports these interventions by reducing fungal load.
However, most established infections require professional treatment for complete resolution, particularly those affecting more than 50% of the nail or present for longer than six months. Home remedies work best as complementary approaches alongside medical treatments or as preventative measures rather than primary therapy for significant infections. Individuals with diabetes, peripheral vascular disease, or immunocompromising conditions should consult healthcare providers before attempting any home treatments.
How long should I try alternatives before considering surgery?
The appropriate treatment timeline depends on infection severity, specific treatments used, and individual patient factors. For prescription oral antifungals, visible improvement typically begins within 3-4 months, with complete resolution requiring the full treatment course of 6-12 months. Topical prescription solutions generally show initial improvements within 4-6 months, requiring consistent application for 9-12 months for optimal outcomes. Laser treatments typically require 3-4 sessions over 3-6 months, with gradual improvement as the healthy nail grows in.
Most podiatrists recommend allowing at least 6-12 months of consistent, appropriate treatment before considering surgical intervention for otherwise healthy individuals. This timeline may be shortened for patients experiencing significant pain, those with severe infections affecting daily activities, or individuals with complicating conditions like diabetes where more aggressive management may be warranted. The key indicator for treatment success isn’t complete cosmetic restoration (which takes 12-18 months as the nail grows out) but rather cessation of infection progression and beginning of healthy nail growth from the base.
Regular reassessment by your podiatrist throughout treatment helps evaluate response and adjust approaches as needed, potentially incorporating multiple modalities to maximize effectiveness before surgery becomes necessary. This systematic approach ensures that surgical intervention, when required, represents a thoughtful progression rather than a premature escalation of care.
| Treatment Approach | Expected Timeframe for Results | Success Rate | When to Consider Alternative |
|---|---|---|---|
| Oral Antifungals | 6-12 months | 70-80% | After 4 months without improvement |
| Topical Prescription | 9-12 months | 50-60% | After 6 months without improvement |
| Laser Therapy | 3-6 months | 60-70% | After full course without improvement |
| Combined Approaches | 6-9 months | 75-85% | After 6 months without improvement |
This timeline serves as a general guideline, with individual treatment plans requiring customization based on specific clinical presentations, patient preferences, and response to initial interventions. Working closely with your podiatrist throughout this process ensures appropriate progression through treatment options. For more insights, you can explore surgical nail removal as an alternative treatment.
Will my toenail grow back normally after surgical removal?
After partial or complete nail removal without matrixectomy, most patients experience regrowth of a new toenail, though the appearance may differ somewhat from the original. Approximately 75-85% of patients develop nails that appear relatively normal, while the remainder may notice some permanent changes in thickness, shape, or attachment to the nail bed. These differences typically become less noticeable over time as the nail continues to mature, with most cosmetic concerns resolving within 18-24 months after surgery.
Factors influencing regrowth quality include the specific surgical technique used, the presence of matrix damage prior to surgery, patient age, and overall health status. Younger patients and those without significant pre-existing nail deformity generally experience better cosmetic outcomes. Following post-surgical care instructions diligently significantly improves the likelihood of favorable regrowth, as does maintaining excellent foot hygiene and avoiding trauma to the developing nail. For those dealing with nail deformities due to fungal infections, understanding nail restoration services can be beneficial.
For procedures involving intentional matrixectomy (destruction of the nail-forming tissue), no regrowth is expected, as this permanent modification prevents nail formation. This outcome, while cosmetically different, eliminates the possibility of recurrent infection in the treated nail and provides lasting relief for patients with severe, recalcitrant cases or significant nail deformity. Most patients adapt well to the nail-free state and appreciate the resolution of pain and infection that previously impacted their quality of life. For those considering alternative treatments, explore options like home treatment vs. professional therapy to manage stubborn nail fungus.